Blood tests can reveal a world of information about your health, but many people overlook the subtle indicators hiding in the numbers. One such parameter is MCHC, or Mean Corpuscular Hemoglobin Concentration. It might sound technical, but understanding it can shed light on your red blood cell health, oxygen transport efficiency, and potential underlying conditions.
This article dives deep into MCHC, breaking down what it is, why it matters, how to interpret its values, and what abnormal results really mean.
What Is MCHC and Why It Matters
MCHC measures the average concentration of hemoglobin in red blood cells. Hemoglobin carries oxygen from your lungs to your tissues, so the density of hemoglobin in each cell directly affects your body’s oxygen delivery.
- High MCHC indicates densely packed hemoglobin in RBCs. This is rare and usually points to inherited conditions like spherocytosis or sometimes lab measurement errors.
- Low MCHC suggests insufficient hemoglobin within RBCs, leading to paler cells and potential fatigue, weakness, or oxygen deficiency.
Calculation Formula:
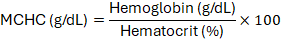
Modern automated analyzers calculate MCHC automatically from the hemoglobin and hematocrit values, but the principle remains the same: it reflects how concentrated hemoglobin is within each red blood cell.
Normal MCHC Values
Knowing the standard ranges helps distinguish healthy readings from concerning trends.
| Population | Typical MCHC Range |
| Adults (male/female) | 32–36 g/dL |
| Newborns | 31–37 g/dL |
| Lab-specific | Minor variations exist based on methods |
Anything outside this range deserves closer scrutiny, preferably alongside other RBC indices like MCV, MCH, and RDW.
Causes of Abnormal MCHC Values
Low MCHC (Hypochromia) Hypochromic red blood cells contain less hemoglobin than normal, appearing paler under a microscope. This can indicate:
- Iron Deficiency Anemia: The most common cause worldwide, resulting from low dietary iron or chronic blood loss.
- Thalassemia Trait: Inherited hemoglobin synthesis disorder.
- Chronic Disease Anemia: Inflammatory conditions may reduce hemoglobin incorporation in RBCs.
- Lead Poisoning or Rare Metabolic Disorders: Occasionally disrupt hemoglobin synthesis.
Symptoms to Watch: Fatigue, dizziness, pale skin, shortness of breath during activity.
High MCHC (Hyperchromia)
Hyperchromic readings are rarer because RBCs have a physiological limit for hemoglobin packing. Common causes include:
- Hereditary Spherocytosis: RBCs become spherical, packing hemoglobin more densely.
- Autoimmune Hemolytic Anemia: RBC destruction can produce unusually concentrated cells.
- Laboratory Artifacts: Cold agglutinins, lipemia, or hemolysis in the blood sample can falsely elevate MCHC.
Warning: Markedly high MCHC is uncommon. Always confirm with a repeat test to rule out lab errors.

How MCHC Fits Into Overall Blood Analysis
MCHC alone is rarely enough to diagnose a condition. Its true value emerges when combined with:
- MCV (Mean Corpuscular Volume): Measures RBC size.
- MCH (Mean Corpuscular Hemoglobin): Indicates hemoglobin amount per cell.
- RDW (Red Cell Distribution Width): Shows variation in RBC size.
Interpretation Examples:
- Low MCV + Low MCHC: Classic microcytic hypochromic anemia (iron deficiency or thalassemia).
- Normal MCV + Low MCHC: Early iron deficiency or anemia of chronic disease.
- High MCHC + spherocytes on blood smear: suggests hereditary spherocytosis.
Combining these metrics provides a clear picture of red blood cell health and helps clinicians decide whether further tests, like iron studies or genetic screening, are necessary.
Lifestyle and Nutritional Factors That Affect MCHC
While many MCHC abnormalities have medical causes, lifestyle and nutrition also play a major role in red blood cell quality and hemoglobin concentration.
- Iron Intake: Red meat, lentils, spinach, and fortified cereals help maintain healthy hemoglobin levels.
- Vitamin B12 & Folate: Essential for RBC maturation. Deficiency can lower hemoglobin concentration per cell.
- Hydration and Exercise: Dehydration may falsely elevate MCHC readings; consistent moderate exercise improves oxygen transport efficiency.
- Chronic Alcohol or Medication Use: Can interfere with RBC production and hemoglobin incorporation, affecting MCHC indirectly.
Focusing on these areas can optimize red blood cell health and prevent mild abnormalities from escalating.
Understanding MCHC in Children and Seniors
MCHC values can vary significantly across age groups, making interpretation age sensitive. Children often show slightly lower hemoglobin concentrations due to rapid growth and higher plasma volume, while seniors may have altered MCHC from chronic illnesses, nutritional deficiencies, or medications. Monitoring trends over time is crucial, rather than relying on a single reading. Regular blood analysis helps detect early anemia, prevent complications, and guide dietary or medical interventions, ensuring red blood cells efficiently transport oxygen throughout the body at all life stages.
Real-Life Example Table: MCHC Patterns
| Condition | MCHC Value | Typical RBC Appearance |
| Iron Deficiency Anemia | 28–32 g/dL | Pale, microcytic |
| Thalassemia Trait | 30–33 g/dL | Small, hypochromic |
| Chronic Disease Anemia | 32–34 g/dL | Normocytic, normochromic |
| Hereditary Spherocytosis | 37–38 g/dL | Spherical, dense |
| Lab Artifact | >36 g/dL | Variable, confirm repeat test |
Conclusion: Take Charge of Your Red Blood Cell Health Today
Your MCHC value is more than just a number—it’s a signal. It can uncover hidden anemia, guide treatment, and reveal early signs of genetic or autoimmune conditions before they become serious. Don’t ignore abnormal values or assume “normal hemoglobin” tells the full story.
Action Steps:
- Request a detailed RBC panel if your MCHC is out of range.
- Monitor trends, not single readings.
- Focus on iron-rich foods, vitamins, and hydration to support optimal RBC function.
- Consult a hematologist if abnormalities persist, especially high MCHC readings.
By understanding and acting on your MCHC results, you take control of your blood health, oxygen delivery, and overall vitality before it’s too late.
FAQs
Q. Can MCHC fluctuate daily?
Minor fluctuations occur, but clinically significant changes usually reflect disease or treatment response.
Q. Is high MCHC always bad?
Not always; sometimes it’s a lab error. Persistent elevation often signals spherocytosis or hemolytic anemia.
Q. Does MCHC measure hemoglobin levels directly?
It measures concentration per RBC, not total hemoglobin in blood.
Q. Can diet alone fix low MCHC?
Only if the cause is nutritional (iron, B12, folate). Other causes need medical evaluation.
Q. Why is MCHC important if hemoglobin and hematocrit are normal?
It detects subtle changes in red cell quality that overall hemoglobin levels may miss.



